Food noise is a term that makes sense to many people. Food noise is a great way to describe the unhealthy way many people think about food, and what they consider to really be food. But, food noise is not the problem, it is only the symptom of a much bigger problem.
Some people can combat and defeat food noise on their own, and some need help...
summerizer
Dr. Ken Barry explains the concept of 'food noise', which is the incessant craving and preoccupation with unhealthy foods. He argues that food noise is a symptom of addiction to sugar and ultra-processed foods rather than a new medical condition. Barry critiques the pharmaceutical industry's response to this phenomenon, proposing that the solution lies not in medications but in dietary changes, particularly eliminating ultra-processed foods and focusing on whole foods, like beef, butter, bacon, and eggs, to break the addiction cycle.
Key Points
Definition of Food Noise
Food noise refers to the persistent cravings and thoughts about food, especially unhealthy options, that individuals experience shortly after eating. Dr. Barry emphasizes that food noise is not a new medical term but rather a symptom of deeper issues related to food addiction.
Marketing of Food Noise
The term 'food noise' gained popularity recently, coinciding with the approval of drugs like Ozempic. Dr. Barry criticizes the introduction of this term as a marketing strategy to promote pharmaceuticals that treat the symptoms rather than address the root causes, such as sugar and carbohydrate addiction.
Nature of Cravings
Barry points out that people generally experience food noise regarding sugary, ultra-processed foods, rather than whole, nutritious foods. He highlights the correlation between these cravings and an addiction to high sugar and carb diets.
Food Industry Manipulation
The video discusses how food manufacturers design their products to exploit human biology, using flavors and ingredients that trigger hunger and suppress satiety, leading consumers to overeat.
Pharmaceutical Solutions vs True Solutions
Dr. Barry warns against relying on pharmaceutical interventions like Ozempic for managing food noise, advocating instead for dietary changes to replace unhealthy eating habits.
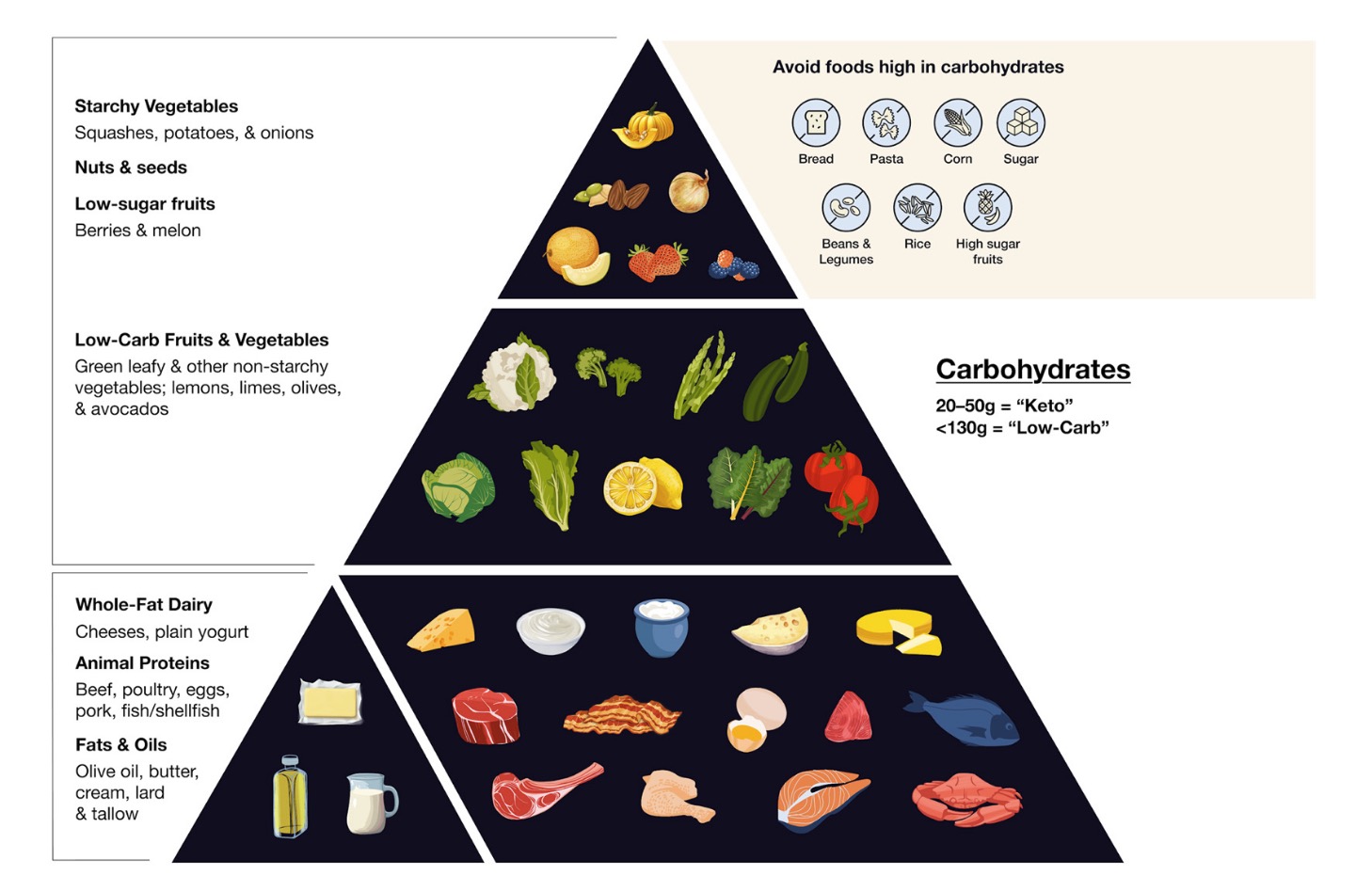
Carnivore Challenge
Barry introduces a 90-day diet challenge of only eating beef, butter, bacon, and eggs, designed to help individuals break free from their sugar and food addiction. The challenge aims to reset hunger and satiety signals in the body.
Long-Term Health Considerations
The speaker emphasizes the risks of long-term pharmaceutical usage for managing hunger and satiety, highlighting the lack of safety research and suggesting that individuals may become unwitting participants in pharmaceutical experiments.
Encouragement for Dietary Change
He urges viewers to consider the dietary changes he proposes not only for personal health improvement but also to assist others suffering from food noise, stressing the large percentage of adults affected by ultra-processed food addiction.